Patients/Carers
The impact of Myalgic Encephalomyelitis (ME) on individuals and families is profound and enduring. For anyone new to ME, the early period - when diagnosis is uncertain or has just been made - can be critical in shaping long-term outcomes. Accurate knowledge during this time is essential for decision-making, particularly for parents of children with ME and for carers of those affected. Below are some details of information about ME that may be useful.

Overview
The impact of Myalgic Encephalomyelitis (ME) on individuals and families is profound and enduring. It is essential that policymakers, the media, and the public approach this condition with accuracy, sensitivity, and respect.
Impact on daily life
ME can cause severe disability, limiting or completely preventing a person from studying, working, or performing everyday tasks such as eating, showering, or leaving bed.
Symptoms such as overwhelming fatigue, pain, cognitive dysfunction ("brain fog"), sensory sensitivities, and post-exertional symptom exacerbation mean that even minor exertion can lead to a serious and prolonged deterioration in health.
Effects on families and relationships
Families often need to reorganise their lives around the needs of the person with ME. Partners, parents, or children frequently act as unpaid carers, which can result in emotional strain, exhaustion, financial pressure, and regret over the loss of previous roles and independence.
Emotional and social consequences
People with ME often experience social isolation due to reduced mobility, limited energy, and misunderstanding of the illness, including stigma or disbelief.
This isolation, combined with uncertainty about prognosis and lack of effective treatments, can contribute to anxiety, low mood, and a sense of abandonment by services.
Educational and employment impact
Many adults with ME are unable to maintain employment or can only work reduced hours, leading to loss of income, job insecurity, and reliance on benefits.
Children and young people may miss long periods of schooling or require home or flexible education, which can affect qualifications, social development, and future opportunities.
Economic and system-wide burden
The economic burden of ME is substantial, with costs arising from lost productivity, informal care, and repeated healthcare contacts, estimated in studies to reach billions when considered at population level.
Under-recognition and under-diagnosis of ME can lead to inappropriate management, unnecessary investigations, and avoidable deterioration, placing further pressure on families, education systems, social care, and health services.
New to ME?
Living with Myalgic Encephalomyelitis (ME, sometimes referred to as ME/CFS) can be incredibly challenging,
not only for those diagnosed but also for their families and caregivers.
Historically, ME has been treated extremely poorly due to neglect, apathy, misinformation and prejudice.
Therefore, support services are still less than optimal and may vary widely.
This is especially so as there is no universally recommended treatment for ME nor are there yet biomarkers for the disease.
For a newcomer (patient, carer, parent) one will need to learn of the support services that are available, both nationally and locally, that may offer limited medical and social assistance.
Below might be a typical, chronological pathway for someone in the UK who may have ME, with the main support options at each stage. (But please read the Disclaimer at the bottom of the page)
- Symptoms: Notice persistent symptoms such as overwhelming fatigue, post-exertional malaise, unrefreshing sleep and cognitive problems lasting at least 6 weeks in adults, and consider keeping a brief symptom and activity diary to show patterns. See NICE Guidelines below.
-
GP Appointment(s): Book an appointment with a GP (likely having been made early on), explain how symptoms limit work, education,
caring and daily tasks, and share any relevant history
such as recent infections or other health conditions.
The initial GP assessment likely includes a physical examination, questions about physical and mental health, and basic investigations such as blood and urine tests to rule out other causes of fatigue.
For GPs ME, without clear biomarkers due to the lack of funding for research, is still largely a diagnosis by exclusion of other conditions. - Advice: Receive early advice on managing activity, rest, sleep, diet and pacing while the GP monitors symptoms over time, even before a firm diagnosis is made.
- Diagnosis confirmation: If symptoms persist for around 3 months and no other cause is found, the individual may be given a working diagnosis of ME based on NICE criteria: disabling fatigue, post-exertional malaise, sleep disturbance and cognitive difficulties that worsen with activity.
- Prognosis: Discuss prognosis and red-flag symptoms with the GP/consultant, including when to seek urgent help if new or concerning signs appear.
- Be referred by the GP (where available locally) to an NHS ME/CFS specialist service or clinic for more detailed
assessment, education and support with symptom management.
Be aware though that there are few ME specialists and consultants who have adequate knowledge of ME, so this may be difficult in some areas. - Ongoing Healthcare Support: Following an offocial diagnosis you may be offered appointments that involve doctors, occupational therapists, physiotherapists and sometimes psychologists focusing on energy management.
- Record: Receive written and verbal guidance on pacing, activity management, rest periods and avoiding post-exertional symptom flares, tailored to severity and daily routine.
- Social Support: Access support for associated symptoms, such as help with sleep hygiene, pain relief, dizziness, and adaptations for cognitive difficulties at home, work or school.
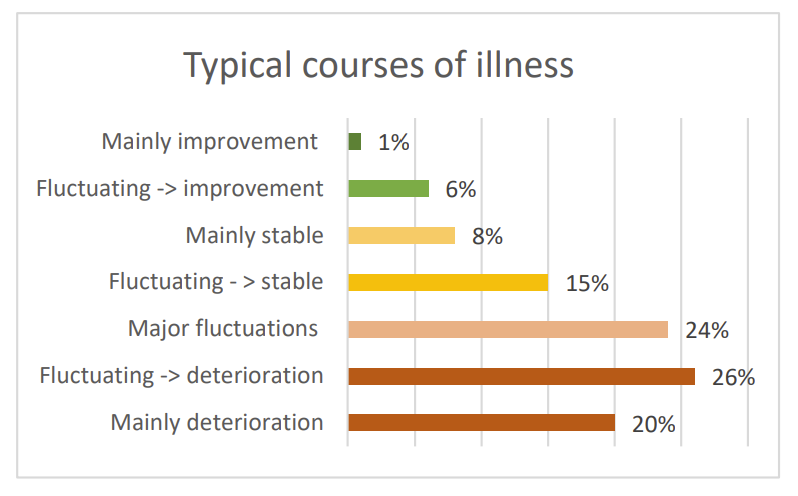
- Severity of ME: Much of what transpires following diagnosis will depend on the course of the illness and how it affects the individual and family.
- Statutory support: such as reasonable adjustments at work under the Equality Act 2010, including flexible hours, home-working, reduced workload and rest breaks.
- Children: For children and young people, obtain support through the school or college,
such as reduced timetable, rest breaks,
home-tuition or blended learning, often coordinated with a paediatric or ME service.
Unfortunately, this can be frustrating as the onus is to have a child back to school as soon as possible (if the school or college has little knowledge of ME) - but it is often the case that a long term view has to be taken. The important point is not to rush a child back to school before they are able to. - Benefits:
Consider applying for welfare benefits such as Personal Independence Payment (PIP), Employment and Support Allowance
(ESA) or Universal Credit health-related elements if daily living and mobility are significantly affected.
This will depend on the current government policy at the time as welfare is a plitical football.
ME is still often misunderstood and DWP exhibits varied attitudes to people with ME, according to our experiences. A useful site is Benefits and Work - Medical evidence: Ask the GP or specialist for supporting medical evidence for benefit claims.
- Social Media and Contacts: There may be a local ME support group or online community some may find useful and that can provide shared experience, See later section on support services.
- Follow-up:
Arrange regular follow-up and contact with the GP and even try to educate them via awareness of IiMER-conferences and
colloquiums and online material.
If using offered specialist services then ensure that they check and review symptoms, adjust management plans and repeat investigations if new issues arise. - Severity: If the condition is severe or very severe, request assessment at home if attending a clinic or GP is not possible, and ask for additional social care input, equipment, and carer support where needed.
Quick reference
- 6yr diagnosis delay
- 400,000 carers
- 0% bedbound peaks
- Employment loss
Links:
Support Services
Access to appropriate support services is critical for improving the quality of life for people living with ME.
It is important to become familiarised with national and any local support services,
including healthcare,
and community support networks.
Some links to the right may be of help
Education
One of the best tools available at present to assist with ME is knowledge - and one needs to become aware of the reality of the situation with ME. Look at the Education page which may have some useful information.
Videos explaining ME science, patient experiences, and research needs for public, media, and healthcare education.
A number of frequently asked questions (FAQs) is given on the right.
Social Media and Contacts
Nowadays, social media can play a useful role for people with ME and their carers.
It can be a valuable source for information as well as interaction with others sharing
the same situation.
Obviously, it can also have its downsides and one has to be aware of individuals and companies
publicisng products that claim to cure or treat ME.
Be cautious of any non-evidence-based “cures” and hype for any product, service or offering. If there was a
magic bullet for ME then this charity would not need to exist.
The charity runs several social media sites and the links are on the right as well as on every web page in the menu or in the foooter.
Local ME Support Groups
There may be a local ME support group or online community some may find useful and that can provide shared experience, pacing tips and emotional support, thus reducing social isolation.
Caregivers play a vital role in supporting individuals with ME, but they also face their own set of challenges.
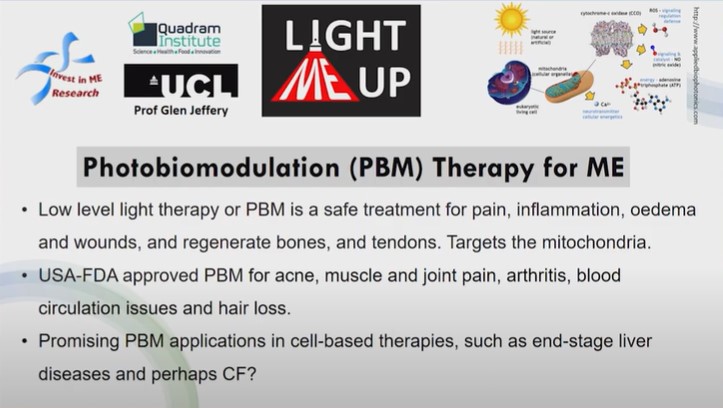
Research
Stay abreast of research developments. Our site has details of the research strategy of the charity and what efforts are being made to provide evidence-based treatments. Our page on a Centre of Excellence also gives information on a strategic approach to research into ME.
News
Keep up to date with current news also. Sign up for the charity newsletter. Read the Journals.
History
If one has further questions, especially on why ME still has no biomarkers or sufficient research then Also our Library section has multiple articles over the last decades.
Conferences
Our annual conferences and colloquia have bring together researchers, clinicians and patient groups regularly from over twenty countries. Videos of the public conferences are available online for free.
Web site
The web site has information so use the links to navigate around.
Get Involved
IiMER's public awareness campaigns attempt to educate and advise on ME in order to remove stigma, educate the media and drive policy change through events, resources, and engagement opportunities. Our Policy page has information for policymakers and the media.
Your MP
Contact your MP and find out what they know of ME.
We have a page of information available for MPs.
Position Statements from the Charity
We have position statements on many of the topics concerning ME, backed up by years of advocacy.
Advocacy Campaigns
Raising public awareness about Myalgic Encephalomyelitis (ME) is a critical step toward improving the understanding of the disease, reducing stigma, and advocating for better treatment and resources. The charity is dedicated to running ongoing awareness campaigns that engage the public, raise visibility, and educate communities on the realities of living with ME. This section highlights the key campaigns and educational resources available to help spread awareness and support.
Despite decades of neglect, support services exist to help people with ME and their caregivers navigate diagnosis, management, and daily challenges through healthcare, community, and statutory support.
Benefits & Adjustments
PIP, ESA, Universal Credit health components. Workplace adjustments (flexible hours, home working). School support (reduced timetable, home tuition) prioritising long-term health over rushed return.
Get Involved
Every breakthrough in ME research starts with people - like us, like you. Whether through a donation, organising a local fundraiser, or joining our research collaborations, your support directly funds biomedical studies that will change lives. No expensive salaries, no waste, direct to making progress.
Your gift funds PhD students, research fellows, medical students, European collaborations, and our work promoting a Centre of Excellence.

Key Facts on Myalgic Encephalomyelitis
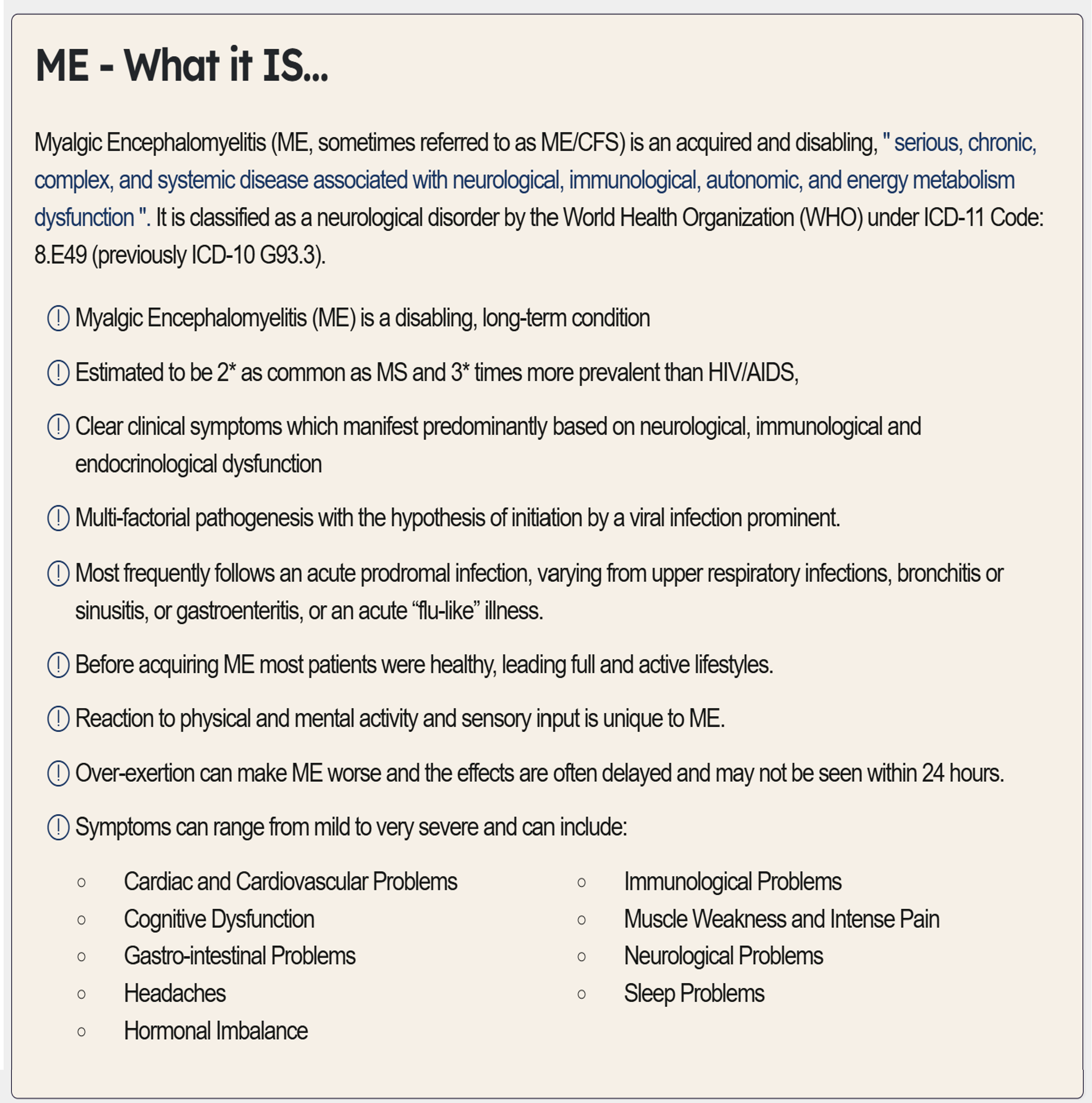
- Myalgic Encephalomyelitis : (ME, sometimes referred to as ME/CFS) - a serious, long-term neurological disease affecting ~400,000+ people in the UK
- WHO Classification: Neurological disorder – ICD-10 (G93.3), ICD-11 (8E49) postviral fatigue syndrome
- Biomedical Reality: Immune dysfunction, autonomic dysregulation, energy metabolism abnormalities, exertion intolerance – not psychological
- Core Symptom – PEM: Post-exertional malaise where minor physical/cognitive/emotional activity triggers delayed, prolonged symptom worsening
- Common Symptoms: Cognitive dysfunction ("brain fog"), unrefreshing sleep, pain, orthostatic intolerance, extreme unrelieved fatigue
- Severity: Significant/severe disability, loss of independence for many patients
- Recognition Gap: Under-diagnosed/under-recognised and under-researched across health/education/social care; long delays, limited specialist access
- NICE NG193 (2021): Rejects GET/CBT as curative; mandates pacing, energy management, personalised support
- Research Priority: Immune dysregulation, viral triggers, autonomic dysfunction, impaired energy metabolism need urgent study
- Historical Context: Decades misclassified as psychological despite clear multisystem biological evidence
- Economic costs: Estimates from £4-7 billion annually
Quick reference
- 400k + UK cases
- £4-7B annual cost
- ICD-11 (8E49) WHO code